Naperville Integrated Wellness
NAPERVILLE'S TOP RATED LOCAL® FUNCTIONAL MEDICINE FACILITY
New Migraine Treatment
We have a new approach to treating migraines, and we are getting great results with it. No, it is not a new drug, dietary supplement or plant recently discovered in a remote part of the world. What we do is address the root causes of dysfunction in the body that result in migraines. Did you know? Serotonin and migraines have a strong connection? Learn more now. If you suffer from migraines, you have probably gone to your primary care physician or maybe even a neurologist and received medication. However, most medications used for migraines address only one possible cause. Medications like Triptans, are a group of drugs that alter how serotonin works in your body; drugs like Imitrex, Relpax and Zomig. A new group of drugs called CGRP antagonists include Aimovig and Ajovy. These drugs primarily affect the nerves. These drugs are believed to block chemical normal nerve activity so that pain signals from the nerves are reduced. In a nutshell, they are an advanced painkiller. Later in this article I will discuss the “migraine nerve” that is responsible for the pain you experience with a migraine. Other drugs may include beta-blockers, antidepressants, anti-inflammatory drugs, antihistamines, etc. As a functional medicine doctor, I look for root causes of health problems. I have found that that there are 3 major factors involved when treating migraines. In this article I will cover the 3 main migraine generators. We will even go one step further and see how they all affect one another. So, there is not a single cause for migraines. If there were, then we would only need one drug and it would work for all migraine sufferers. Let’s start with how a migraine occurs… Older theories about migraines suggested that symptoms were possibly due to fluctuations in blood flow to the brain. Now many headache doctors and researches realize that changes in blood flow and blood vessels don’t initiate the pain, but contribute to it. Today, it is widely understood that chemical compounds and hormones, such as serotonin and estrogen, often play a role in pain sensitivity for migraine sufferers. When serotonin or estrogen levels change, the result for some is a migraine. Serotonin levels may affect both sexes, while fluctuating estrogen levels affect women only. https://www.hopkinsmedicine.org/health/conditions-and-diseases/headache/how-a-migraine-happens These 3 natural and beneficial chemicals are most commonly involved in migraines. You can’t alter one of these chemicals without affecting the others and the end result is that it triggers a very important nerve. I call this the “migraine nerve” and it is responsible for pain you experience with a migraine. “Migraine is a predominantly female disorder. Menarche, menstruation, pregnancy, and menopause, and also the use of hormonal contraceptives and hormone replacement treatment may influence migraine occurrence. Migraine usually starts after menarche, occurs more frequently in the days just before or during menstruation, and ameliorates during pregnancy and menopause. Those variations are mediated by fluctuation of estrogen levels through their influence on cellular excitability or cerebral vasculature.” The Journal of Headache and Pain https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3311830/ “Biochemical evidence suggests central and peripheral roles for estrogen in the pathophysiology of menstrual migraine, and interactions with serotonergic (serotonin) components.” This means estrogen itself is involved in the cause of migraines but it also affects how serotonin works, which will also contribute to migraines. Journal of the American Medical Association https://jamanetwork.com/journals/jama/fullarticle/202685 Serotonin is a chemical that affects our blood vessels, our mood and how we perceive pain. Serotonin migraines can cause blood vessels to contract or relax. A common medication used to manage migraines is Imitrex and it binds to specific serotonin receptors that cause the blood vessels in your head to constrict. “Sumatriptan (Imitrex) binds strongly to serotonin 5-HT1B/1D receptors and is thought to relieve migraine symptoms through an inhibition of pro-inflammatory substances and a constriction of cranial blood vessels.” This demonstrates the importance of proper balance and function in the body. It helps regulate blood vessels and reduces inflammation. So what can we say about serotonin and migraines? They are connected. https://www.drugs.com/tips/sumatriptan-patient-tips The nerve that carries the pain signals of a migraine is called the trigeminal nerve. You have 2 of these nerves, one from the left side Estrogen and serotonin play a significant role in migraines. The trigeminal nerve carries the pain signals from the affected blood vessels to the rest of your brain and that is how you experience or feel the pain of the migraine. So, I am calling the trigeminal nerve the “migraine nerve.” You could not experience pain from a migraine without this nerve. This nerve has receptors for estrogen and serotonin…meaning they influence how this nerve works and how you feel the pain of a migraine. “Estrogen acts as a neurosteroid influencing the pain pathway associated with migraine by binding to its receptors (estrogen receptors) present on the trigeminal nerves. The trigeminovascular system consists of a network of cranial blood vessels and their trigeminal innervations that convey the pain information to the central nervous system where migraine pain is perceived. Decreased levels of a neurotransmitter serotonin, are also linked to migraine. The implication of serotonin in migraine has been indicated by studies showing the presence of its receptors (5-HT receptors) on the trigeminal nerve and cranial vessels and also by the relief obtained after serotonin administration.” Annals of Neurosciences https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4117063/ “Histamine has been known to cause a vascular type headache (migraine) for almost a hundred years.” The Journal of Headache and Pain https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-019-0984-1 “Histamine-induced headache is a vascular (blood vessel) headache. In migraine patients, plasma histamine concentrations have been shown to be elevated both during headache attacks and during symptom-free periods.” The American Journal of Clinical Nutrition Histamine is the chemical that causes the symptoms associated with allergies…itchy eyes, runny nose, etc. but that is only one of many functions of histamine in your body. It is a chemical that is involved in the function of the immune system, but it also acts as a There are histamine receptors in blood vessels, the brain and nerves that carry pain signals. Histamine will increase pain signals while serotonin tends to decrease pain signals in the body. “The pain caused by the trigeminal nerve has been described as the most agonizing known to humankind…” https://www.theguardian.com/lifeandstyle/2011/oct/17/mapping-the-body-trigeminal-nerve If you do not make enough of the enzyme (DAO) to breakdown excess histamine in your body, you may experience a migraine. The health of your digestive system will also influence your ability to breakdown histamine, the preventing a migraine. Many of the foods listed as “migraine triggers” are foods and drinks that are high in histamine or cause your body to release too much histamine, triggering a migraine. In our office we often discover that migraine sufferers have some degree of histamine intolerance. This means they have difficulty breaking down excess histamine. This is how diet can play a significant role in the treatment of migraines. “Hence, histamine release and accumulation in the trigeminal nerve plays an important role in the pathogenesis (cause) of neuralgia (nerve pain). Journal of Oral and Maxillofacial Research When the 3 factors leading to a migraine are assessed and addressed, most of our patients who suffer with migraines experience significant improvement or the elimination of migraines entirely. There is no medication that addresses these 3 causes. Some address serotonin, some address the pain, some address inflammation, some address how blood vessels work, etc. In functional medicine we look for the root cause of migraines. As you now see, it can be due to various chemical imbalances. Each of these 3 main factors are medically recognized causes of migraines, but they are not being addressed nor or doctors recognizing how all estrogen, serotonin and histamine all influence each other. So what makes our treatment new is that we are not just focusing on a single cause, nor are we trying to suppress the results of these causes (like inflammation). We are addressing the root cause of migraines so that our patients can have far fewer migraines, less debilitating migraines and many cases, no migraines at all. We are achieving this without the use of drugs and most of our patients are able to reduce or eliminate the migraine medications they were taking. How a Migraine Happens…
3 chemicals that cause migraines
Estrogen—Serotonin—Histamine
“migraine nerve”
Estrogen
 Why more women get migraines than men…
Why more women get migraines than men…Estrogen alters how serotonin and histamine work in your body…
 Serotonin and migraines…
Serotonin and migraines…Why you feel pain…
“migraine nerve”
 of your brainstem and one from the right.
of your brainstem and one from the right. Histamine
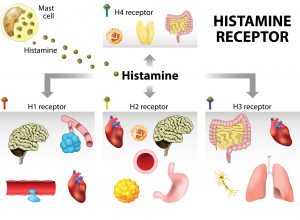 neurotransmitter (serotonin is also a neurotransmitter).
neurotransmitter (serotonin is also a neurotransmitter). Food Triggers
Aggarwal, M., Puri, V., & Puri, S. (2012). Effects of estrogen on the serotonergic system and calcitonin gene-related peptide in trigeminal ganglia of rats. Annals of Neurosciences, 19(4), 151-157. Retrieved 10 23, 2020, from https://ncbi.nlm.nih.gov/pmc/articles/pmc4117063
Brandes, J. L. (2006). The Influence of Estrogen on Migraine: A Systematic Review. JAMA, 295(15), 1824-1830. Retrieved 10 23, 2020, from https://jamanetwork.com/journals/jama/fullarticle/202685
Chai, N. C., Peterlin, B. L., & Calhoun, A. H. (2014). Migraine and estrogen. Current Opinion in Neurology, 27(3), 315-324. Retrieved 10 23, 2020, from https://ncbi.nlm.nih.gov/pmc/articles/pmc4102139
Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American Journal of Clinical Nutrition, 85(5), 1185-1196. Retrieved 10 23, 2020, from https://academic.oup.com/ajcn/article/85/5/1185/4633007
Sacco, S., Ricci, S., Degan, D., & Carolei, A. (2012). Migraine in women: the role of hormones and their impact on vascular diseases. Journal of Headache and Pain, 13(3), 177-189. Retrieved 10 23, 2020, from https://ncbi.nlm.nih.gov/pmc/articles/pmc3311830
CONTACT
Call: (630) 210-8391 or fill out the form below
"*" indicates required fields
